Kids Sleep Disordered Breathing (SDB)
As parents we want to give our children the best opportunities to succeed in life. What if something as simple as breathing could be interfering with your child’s success? Sleep Disordered Breathing (SDB) is an all–inclusive term for breathing difficulties, ranging from mild snoring to a severe obstruction during sleep (sleep apnea). When your child’s breathing is disrupted, his or her body recognizes the disruption much like choking, therefore, slowing the heart rate, raising the blood pressure, arousing the brain, ultimately disrupting sleep. This prevents proper brain function for the next day and often leads to several medical complications.
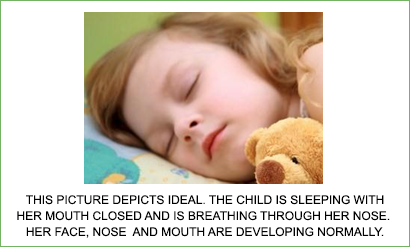

The child on the LEFT is sleeping with her mouth open.Note the already protruding upper anterior teeth and the chapped lips. She is mouth breathing. The inspired air is not being properly warmed, humidified and filtered. She is developing an open bite, improper anterior tongue thrust swallow, and a narrow upper arch. She may or may not have obstructive sleep apnea, but this is not a healthy pattern.
There are many visual signs we are trained to see that can help aid in furthering a diagnosis.
Signs & Symptoms
Unfortunately, 9 out of 10 children suffer from one or more symptoms of sleep apnea. Symptoms like ADHD/ADD, bed-wetting, night terrors, poor school performance, snoring and mouth breathing are just some of the outer signs of the underlying root cause. These symptoms do not self-correct. In fact, 92.6% of children will continue to exhibit these symptoms throughout their life and 30% will worsen with age.
The Silent Crisis Among Children
ADD/ADHD
Bed Wetting
Difficulty in School
Mouth Breathing/Snoring
Restless Sleep
Delayed or Stunted Growth
Nightmares
Irritability/Anger
Morning Headaches
Chronic Allergies/Eczema/Asthma
Depression
Tooth Grinding
Swollen Adenoids/Tonsils
Aggressive Behavior
Daytime Drowsiness
Peer Problems/Few Friends
Frequently Wakes Up at Night
Sleep Talking/Walking
An Estimated 9 out of 10 kids Suffer from One or More of These Symptoms
Frequently Asked Questions:
Whats wrong with Mouth Breathing?
Many children breathe through their mouth during the day and at night. One of the functions of the nose is to warm, moisturize and filter the air before it gets to our lungs. Mouth breathing doesn’t do this and the air is more likely to enlarge the tonsils and irritate your lungs. Some people constantly breathe through the mouth because of chronic nasal congestion, enlarged tonsils and adenoids, abnormal size of the jaws or an anatomical abnormality in the nose. While asleep with your mouth open, the lower jaw has a tendency to fall back and constrict the airway. This causes less oxygen to be delivered to the brain, the muscles and all the cells of the body; therefore, the body functions less than optimally.
Breathing through the mouth can also dry the oral cavity, lead to bad breath, cause crooked teeth, tooth decay, gum disease, poor growth and/or facial deformities. Children who breathe through the mouth at night may snore and have a restless sleep. They often wake up tired, irritable and have dark circles under the eyes. When a child is not able to breathe well while sleeping it can affect the brain and body’s growth and development.
Is Snoring normal?
Snoring is common, it may be cute but it’s NOT normal! The noises produced by snoring are caused by a blockage in the flow of air that reaches the body when breathing. This could be caused by poor tongue posture and the shape of the nose or the jaw. When the body doesn’t take enough oxygen, the brain sends a signal to the body to wake up to get oxygen. The most common symptoms children with compromised airway face are: difficulty listening, chronic allergies, fidgeting, restless sleep, teeth grinding, ADHD, and bedwetting.
Why is my child still wetting the bed?
Bed-wetting is a common symptom of Sleep Disordered Breathing and in fact, almost 1 in 5 children, grade school age, quietly suffer from bed-wetting. When the brain has a lack of oxygen it can cause a slack in the control of bodily functions. This creates anxiety, guilty feelings and can disrupt family life.
Could there be other reasons for my child to exhibit ADHD/ADD and other behavioral problems?
Did you know that, according to research, Sleep Disordered Breathing increases the risk of being diagnosed with ADD/ADHD by at least 50%? Unfortunately, many of these children are misdiagnosed and put on medication. Before heading down the medication path, every parent owes it to their child to have their airway assessed. Children who can’t sleep properly are often tired, irritable and may exhibit aggressive behavior.
Can some learning difficulties be a result of lack of good sleep?
REM-sleep is especially important during early childhood development. Lack of REM sleep has been shown to impair the ability to learn complex tasks. During this time, signals are sent to the brain’s cerebral cortex which is responsible for learning, thinking and organizing information. Snoring and mouth breathing are signs that a child is struggling to breathe, typically due to an obstructed airway. Lack of oxygen to the brain keeps the body from experiencing REM-sleep. Children without proper REM-sleep may have trouble in academic subjects like math, science, reading and spelling.
What is the solution?
We now have the ability to identify these issues and provide a solution for sleep apnea. After a thorough review of the medical history and a dental examination, if the root cause of these problems is of dental nature, an appliance therapy may be indicated to properly position the upper and lower jaw relative to each other and to the bones of the face. Depending on the diagnosis, we can make an appropriate appliance or we can refer to a specialty orthodontist or a myofunctional therapist. The ultimate goal is to promote an open airway, proper growth of the jawbones, better tongue position, proper nasal breathing and eliminates bad oral habits. If the root cause is medical, the most common cause is enlarged tonsils and adenoids which can be treated by a medical doctor.